This piece was first published by the Wentworth Courier.
The Emergency Department at St Vincent’s Hospital in Sydney is quieter than usual, which is strange considering we are in the midst of a pandemic. This is an inner-city emergency department that just six weeks ago was treating two hundred people per day. The numbers are currently half that, according to the department director, Dr Paul Preisz. Doctors and nurses on the ward describe the atmosphere as eerie but better than the alternative.
“It’s quiet and that’s bad. We shouldn’t be saying that,” says registered nurse, Erin Macdougall.
Emergency ward superstition says that uttering the q word will reverse your fortune.
Faced with an increasing number of COVID cases in Australia, the federal government implemented strict physical distancing and isolation regulations to stop the spread of the virus. This allowed hospitals to prepare for the pandemic and reduce the chance of being overwhelmed by an influx of patients.
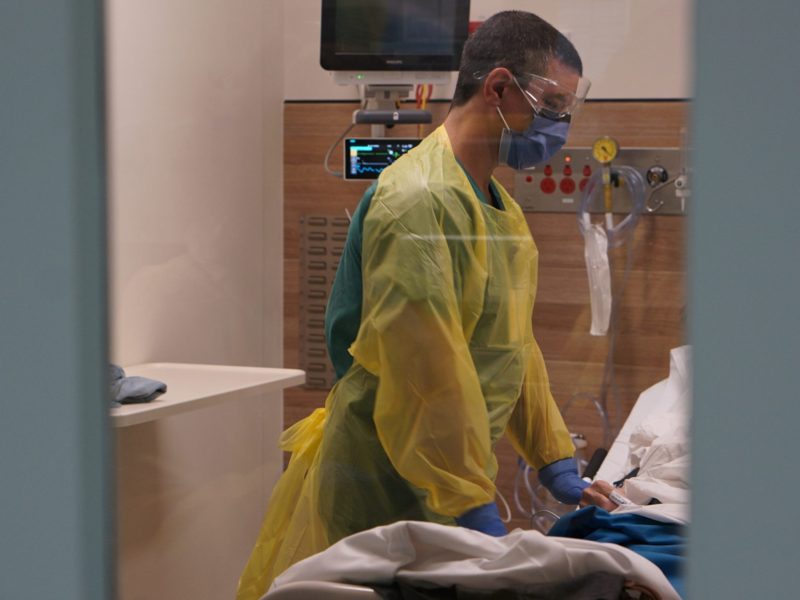
At St Vincent’s they established an Emergency Operations Centre responsible for dealing with the outbreak. They created new COVID-specific procedures and rosters, cross-trained staff on intubation, and sourced personal protective equipment. They redesigned their brand new $17.5 million emergency department and its state-of-the-art facilities to accommodate a quarantine zone for any new arrivals who they suspect of having COVID-19 and they decentralised their testing hub by establishing a drive-through centre at the Bondi Pavilion. They achieved all this in roughly six weeks thanks to a large amount of hard work and government cooperation.
“The government reacted well in the sense that we were given pretty much everything we needed…We were not irrational. I think everyone was very cautious and bought what we needed to face this,” says Dr Gonzalo Aguirrebarrena, deputy director of St Vincent’s Emergency Department.
Where before emergency staff were worried about how the hospital would cope with an overwhelming number of patients, now they feel more at ease.
“I was really terrified at the start, more of us being unprepared, not of me catching it…I feel like we’ve worked a lot and I feel much more prepared and much more organised,” says Macdougall.
Emergency staff have been following strict physical distancing measures which keep them away from loved ones and family. For registrar, Elle Corrigan, this isolation period “feels like a lifetime.” Another registrar, Eva Rosenbaum, had planned to take a year off from medical work after feeling burned out. She’s now back at the hospital working in emergency.
Dr Preisz believes the government’s plan to stop the spread of the virus has been effective so far. The number of new cases in NSW is dropping every day. Indeed, at the time of writing, there was one COVID patient in intensive care and a few in the ward. Two weeks ago, there were 30 or 40 new cases presenting to the hospital and its screening clinics each day.
An unexpected outcome of the physical distancing and isolation restrictions is a quiet emergency department. It is hard to say whether that is because members of the public are avoiding hospitals and emergency departments or that less activity due to the regulations means fewer accidents; possibly a combination of the two. The upside to this is that people with less serious conditions aren’t occupying valuable emergency beds. The downside is that patients who need medical attention might not be receiving the care they need.
While emergency personnel are appreciating a reduced workload, they remain worried that the country is susceptible to a bad outbreak.
“It doesn’t matter how prepared we are here, how many nurses, ventilators we’ve got…If the community is not doing their part and staying at home, isolating and quarantining, then this is all for nothing,” says registered nurse, India Wells.
Health authorities now have a conundrum. The efficacy of our restrictions means a large percentage of the population are not infected and are susceptible to the virus. Yet the moment the authorities relax the measures there might be some spread of the disease. Without a vaccine in sight, it appears the state and federal governments will be playing a balancing act for the foreseeable future.
For now, the messages from government remain clear: isolate, physically distance, minimise unnecessary travel. How long this will go on for is unclear. The healthcare workers at St Vincent’s remain on edge knowing full well that this could just be the calm before the storm. At the very least, it’s comforting to know we are prepared for the worst.
“We don’t know whether it will happen or not, but you’ve got to prepare for it. You have no choice,” says Dr Preisz.